News

Minimally invasive bioprinting
Researchers in the MIRACLE II team at the University of Basel are focused on new technologies to enable minimally invasive medical interventions. As part of this work, they’ve now taken the first steps towards developing a 3D bioprinter that could one day print artificial tissue directly into an operation site.
Bioprinting is widely viewed as the future of medical technology. The idea is to use biological substances—so-called bio-inks—to print three-dimensional structures that imitate natural tissues. In surgical interventions, bioprinting technology could be utilised in various ways—for instance, to inject new tissue into a wound after an operation. And already today, simple tissues like muscle, cartilage or skin can be printed and used for testing new drug therapies.
Bioprinters that facilitate minimally invasive surgeries would be particularly interesting. Indeed, surgeons are increasingly choosing minimally invasive techniques, as they cause less damage to surrounding, healthy tissue. The robot-guided laser system to enable minimally invasive bone surgery developed in the WSS-funded MIRACLE II project supports this trend.

Finding the right consistency
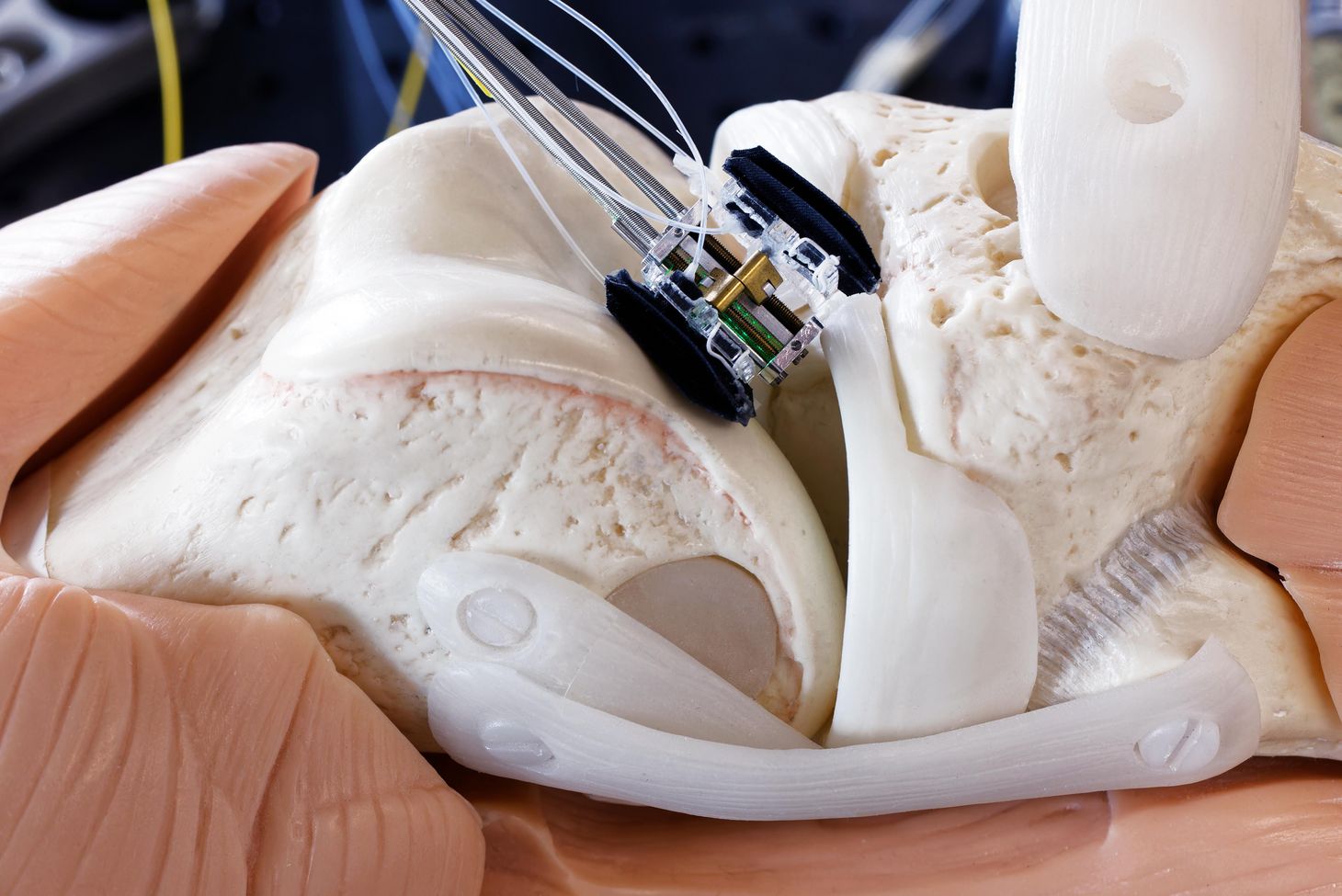
And now, researchers in the project team have taken the first step towards constructing a minimally invasive bioprinter. They began by building an experimental bioprinting platform in order to find out which factors influence the printing behaviour of a bio-ink and in what ways. Georg Rauter, project leader and robotics specialist from the BIROMED Lab at the University of Basel, says this work was conducted as part of a master’s degree thesis that focused on cartilage replacement in the knee joint—to help patients with osteoarthritis, for instance.
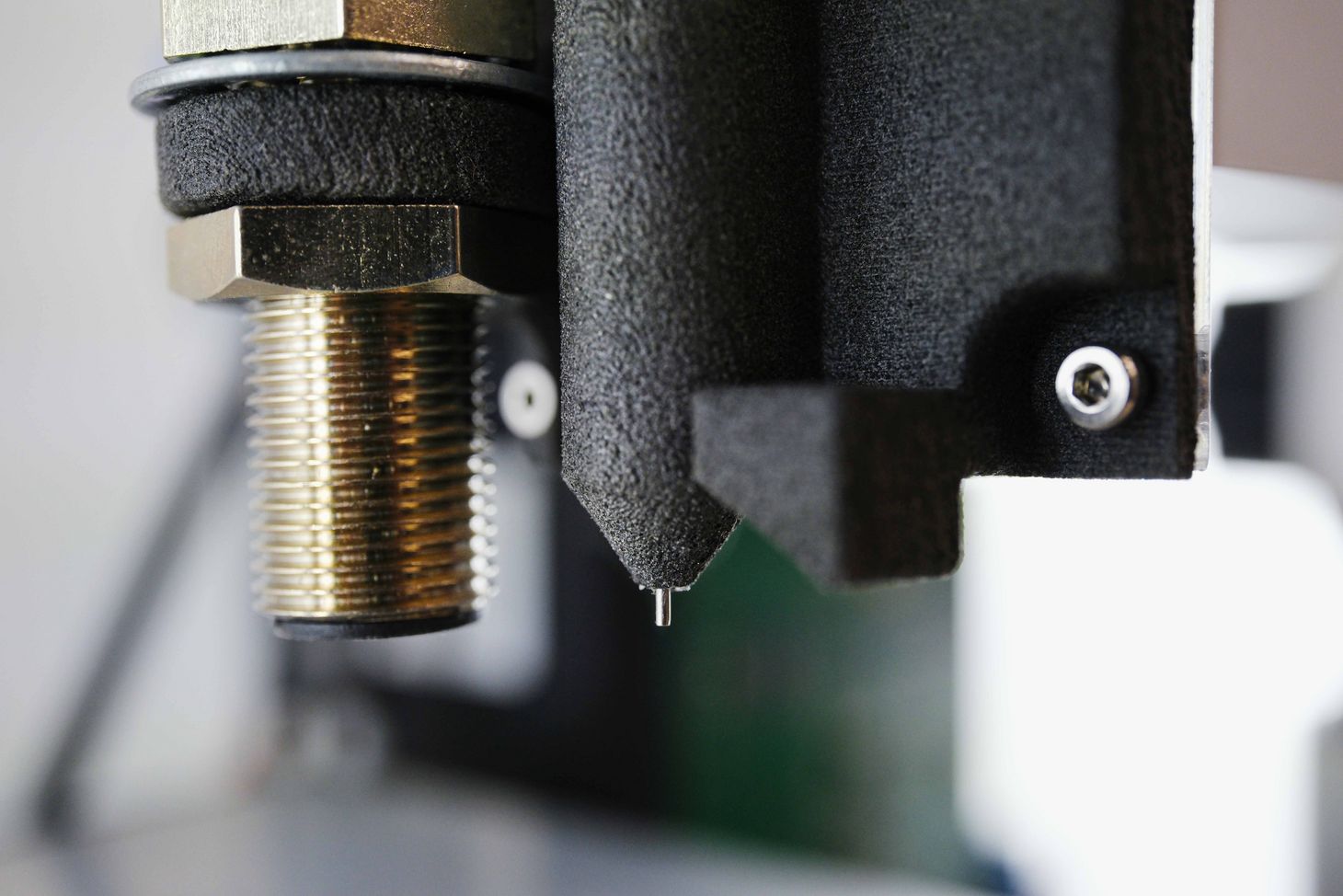
In regenerative cartilage medicine, so-called hydrogels are used as the printing material, Rauter explains. In their experiments, the MIRACLE researchers chose a hydrogel called gelatine methacryolyl, which they heated to various degrees and then tested for how it reacts when exposed to pressure from tubes and nozzles of different sizes. “The key to success is finding the right consistency for the hydrogel so that a continuous, reproducible material flow is possible,” Rauter explains.
A study recently published in the science journal “at – Automatisierungstechnik” demonstrated that a filament suitable for printing 3D structures can be formed using the new platform. But while confirmation that the principle of injecting hydrogels into the body via a thin tube is indeed promising, the researchers still have much to do before the system is viable. One open task is integrating a method for hardening and stabilising (known as “linking”) the hydrogel after printing.
Hard to harden
“This linking occurs differently, depending which printing material we choose,” Georg Rauter says. Hydrogels are often admixed with very specific molecules; after printing, exposure to light or heat can change these molecules, causing the hydrogel layers to stiffen and cross-link. Finding the right kind of molecule, adding the right amounts and choosing the right exposure techniques are among the main challenges facing the team, as Rauter explains.
The researchers also need to find a way to control the hydrogel’s correct, printable consistency even in an emergency. A complicating factor is that—depending on where the operation site is—shorter or longer tubes are used to introduce the bio-ink into the body, but warming the bio-ink or maintaining its temperature inside a tube can prove difficult, as there is little room inside the human body for insulating the tube or otherwise keeping it warm.
In the project’s next step, Rauter and Florian Thieringer, professor and senior physician for oral and cranio-maxillofacial surgery and head of the inhouse 3D printing lab at the University Hospital Basel, plan to recruit a PhD student to work on the minimally invasive bioprinter. Rauter says he hasn’t yet succeeded in winning a grant from the Swiss National Science Foundation (SNSF) to fund a larger research project. “Right now, we’re working on a tight budget, without the necessary financing. But we believe the method has huge potential.” One that could later find use in the technology for minimally invasive bone surgery being developed in the MIRACLE II project.
> Link to study