News
Smart laser scalpel
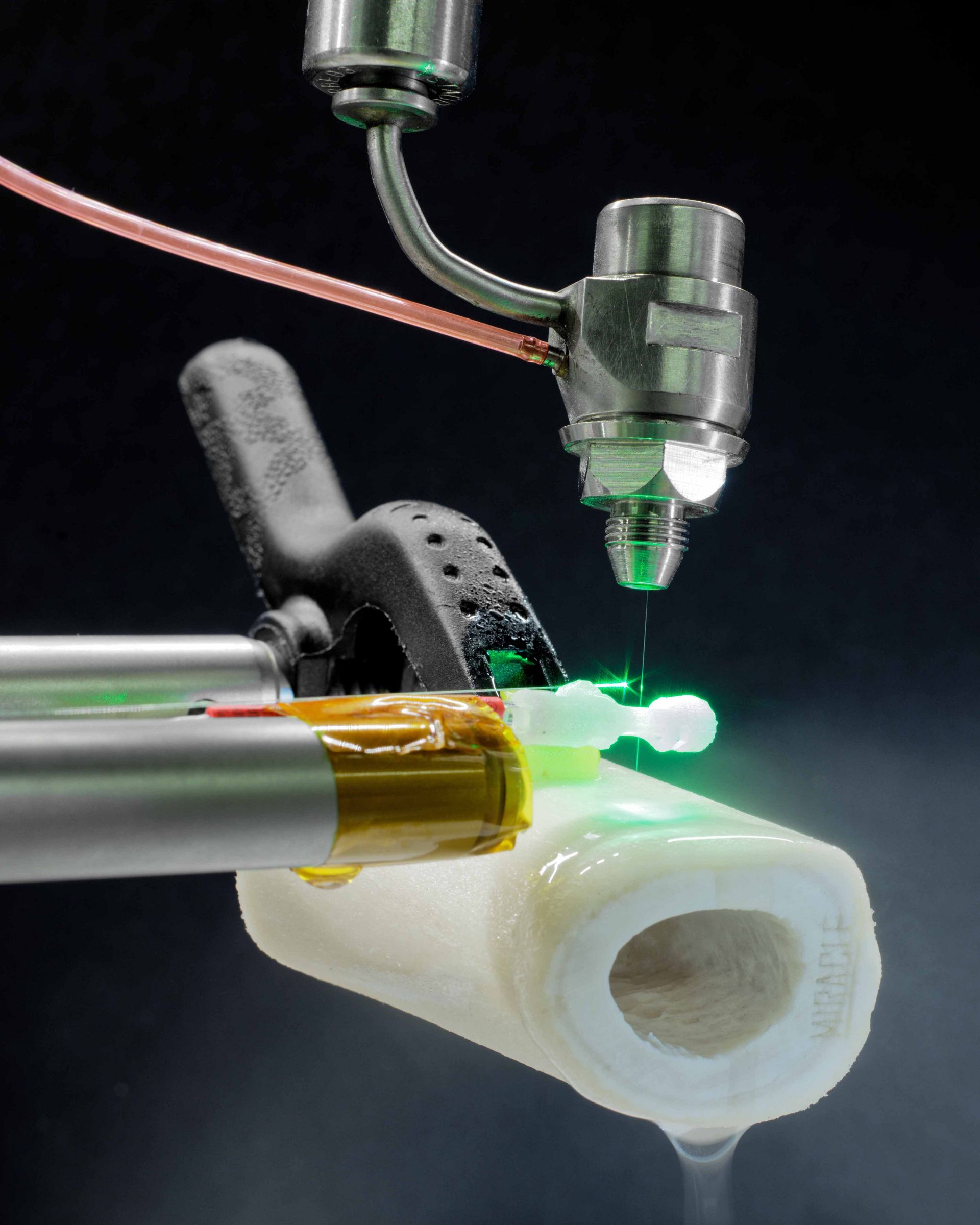
Forget the bone cutter—get ready for the laser scalpel: researchers from the MIRACLE project are working to make minimally invasive bone surgery a reality. Their robot-guided laser system makes fine, precise incisions and—thanks to newly developed sensors—can monitor its own incisions and ensure patient safety.
Today, abdominal and joint surgery is routinely performed using minimally invasive procedures. Rather than making large incisions through skin and tissue, surgeons access the operation site by inserting endoscopes into the body through tiny incisions. These procedures are much less traumatic for the patient: wounds heal more quickly and recovery time is faster. That is why the MIRACLE project team, led by professors Philippe Cattin and Hans-Florian Zeilhofer at the University of Basel, want to make minimally invasive surgery possible on bones, too—using a robot-guided laser beam. Their “laser scalpel” makes extremely fine and precise incisions in bones, and is able to cut in straight, curved and S-shaped lines. Broken bones can be fitted together again like three-dimensional puzzle pieces, allowing them to knit faster.

Smaller size, greater control
The research team in Basel are moving ever closer to their goal of developing a laser scalpel for minimally invasive bone surgery. They are currently working on two fronts: first, the laser components developed to date must be made smaller to fit into the endoscope tip; second, miniaturised sensors must be placed at the endoscope tip in order to continually measure the exact location of the laser scalpel during an intervention. “During endoscopic procedures, surgeons can’t directly see what’s happening in the body, so we need technologies that aid navigation,” says Philippe Cattin. To this end, the researchers have developed new optical sensors to be inserted into the flexible, robot-guided joints of the laser endoscope tip; the sensors record the angle of the joint and thus the movements of the endoscope. Cattin holds up an approximately one-centimetre large sensor and explains: “Electric components and tiny mirrors are positioned inside the sensor so that they can make extremely precise measurements of angles. It already functions in principle. Now we have to make the sensors just a little smaller so that they fit into the joints of the laser endoscope tip.”

Tiny and reliable
Professor Georg Rauter, head of the project’s robotics group, shows how the laser scalpel is situated at the endoscope tip—the actual heart of the system is a bona fide robot in miniature. On its sides are two “arms” that can latch on to the bone for stability and precision; recent tests have demonstrated that the tiny robot can perform precise movements down to at least the quarter millimetre. But the laser can do more than cut—the MIRACLE laser physicists have created a true multitalent. Using Optical Coherence Tomography (OCT), the laser scalpel simultaneously measures the depth of an incision while cutting. The system can also characterise tissue: depending on the type of tissue, the laser light produces different light emissions and acoustic signals that are then measured by the system to determine whether the laser is cutting through bone, nervous tissue, healthy tissue or a tumour. Combined with the OCT method, which also delivers information on tissue type, the technology works already shortly before the laser starts cutting. “This way, we can convert a laser beam that, in principle, would cut indiscriminately through anything and everything into a smart and safe system that only severs the targeted tissue,” says Professor Azhar Zam, head of the Biomedical Laser and Optics Group. One challenge lies in integrating the laser light at the endoscope tip, as standard laser sources are far too large to fit into an endoscope. As such, the considerable laser energy required to cut through bone must be generated either by a much smaller source or externally via a thin glass-fibre cable inserted in the endoscope tip. The various approaches under consideration by the laser physicists are now being further developed and tested in order to determine the best method.
Better surgery planning
The researchers have also further developed SpectoVR, their successful virtual reality software that aids doctors in planning operations. The system transforms CT or MRI scans into virtual, three-dimensional images that can be explored using data goggles. “It makes surgical planning simpler and more intuitive,” says Cattin, “and the feedback from doctors already using SpectoVR is very positive.” But the team have still greater ambitions: the next goal is to integrate haptic rendering capabilities into the system, enabling doctors not only to see in 3D, but also to touch virtual objects in the simulated environment. The prototype, which has already been constructed in Georg Rauter’s robotics lab, is now being further developed. Progress is well underway: users can already use a stylus to “feel” a backbone in the virtual environment. Using haptic technology, the software renders the original CT images, generating the right amount of resistance for each point touched—so that the virtual copy feels like a real vertebra. The system is a global first and extremely useful: in addition to allowing surgeons to plan operations even more precisely, the haptic experience is designed to improve surgical training. “We envision future surgeons using a virtual 3D model to practise precise drilling techniques on bones,” says robotics engineer Georg Rauter. Based on its considerable successes, the MIRACLE project will receive a grant from the Werner Siemens Foundation for a second phase starting in 2022.
Text: Santina Russo
Photos: Oliver Lang