Drug and immune booster in one
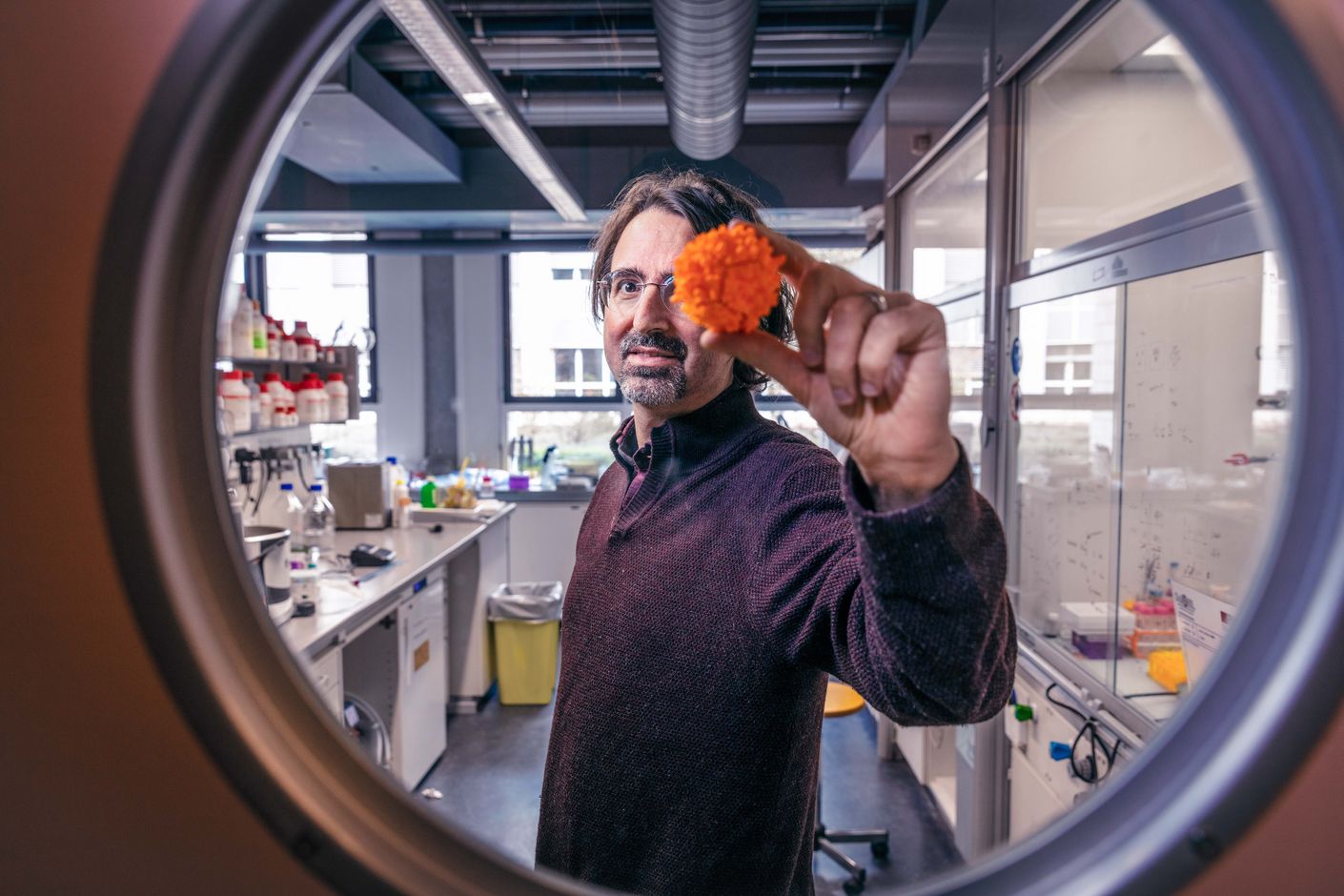
We use drugs to kill pathogens and vaccines to help our immune systems ward off infection in the first place. Now, researchers in the team led by Francesco Stellacci at EPFL in Lausanne have developed a medication that does both at the same time.
AIDS, Covid-19, influenza, hepatitis, measles, mumps, yellow fever—there are numerous kinds of viral infections. Some are relatively harmless, while others are life-threatening. But what they all have in common is that they replicate by invading host cells in the human body, where they reprogram the cells to begin producing and releasing new viruses.
Up to the present day, however, developing effective antiviral drugs has posed major difficulties to medical researchers. One problem is that medications soon lose their efficacy due to a virus’s uncanny ability to adapt and mutate rapidly. Another is the long-held belief that the best way to fight a virus is by stopping its reproduction inside a cell, an approach that bears a risks of side effects.
A team of researchers led by Francesco Stellacci at the Supramolecular Nano-Materials and Interfaces Laboratory of EPFL Lausanne are tackling the problem from a different angle. In their project, which is financed by the Werner Siemens Foundation (WSS), they are developing antiviral agents that attack a virus before it has a chance to enter a cell and multiply. Their method is based on modifying a specific type of sugar molecule—cyclodextrins—with several water-repellent chains of carbon and hydrogen atoms.
Pressure on the viral envelope
These finger-like protrusions attract viruses, bind themselves to them, and then exert such strong mechanical pressure that the viral envelope is permanently damaged. In contrast to conventional antiviral drugs, the new development not only prevents viruses from replicating: it also effectively and irreversibly destroys them. The viral remains are then disposed of in the body by the immune system. Because all the action is extracellular, the human cells themselves remain intact and unchanged. Studies have already shown these kinds of agents to be promising against various viral infections.
Now, Stellacci and his team have enhanced this principle with a very clever feature: in a study (*) recently published in the peer-reviewed journal Small, the researchers created a novel antiviral agent using an already existing peptide: Pam3CSK4, a so-called lipopeptide with three water-repellent appendages. “Its structure is similar to the cyclodextrins we use as antiviral agents,” Francesco Stellacci explains.
The researchers augmented the Pam3CSK4 with four short peptides that dock on to the viral attachment ligand of an influenza virus called “haemagglutinin”, which is a protein that allows the flu virus to attach itself to a human cell—the first step before it enters a cell to replicate. The study demonstrated that the peptide-enhanced lipopeptide prevented the virus from entering the cell—and that it’s capable of destroying the virus.

Stimulated immune system
And there’s more, as Francesco Stellacci explains: “Pam3CSK4 is known for its ability to stimulate the immune system.” The lipopeptide ensures the maturation of so-called dendritic cells, which in turn can induce a primary immune response, meaning the body’s immunological reaction when it first comes into contact with a new pathogen. “The question arose as to whether Pam3CSK4 would still recruit immune cells after our modification,” Stellacci relates.
And in fact, the modified molecule, which the researchers named Pam3FDA, did indeed perform a dual function: it has an antiviral effect in that it irreversibly prevents flu viruses from entering a cell, and also an immunisation effect in that it stimulates the immune system.
Stellacci believes this combination is a novelty: “We haven’t found any drugs that work with this dual effect.” He also says that this way of functioning is precisely what makes a good antiviral agent—because a drug that blocks or eliminates every single virus wouldn’t be successful in the long run: “If someone is re-infected, the whole procedure would have to start all over again.” A better idea is a medication that helps keep a pathogen in check while simultaneously preparing the immune system for a potential re-infection.
Avoiding overreactions
Stellacci points out that this kind of a “two-fisted” agent isn’t the right choice for treating all viral diseases. Indeed, some infections are dangerous because they trigger the immune system into overreacting, which results in the body attacking itself. “In these cases, our drug isn’t a good fit because it would further stimulate an already over-active immune system,” he explains. Here, a cyclodextrin-based drug without an immunostimulant effect would be more promising.
The combined preparation, however, has potential in the case of respiratory viruses, Stellacci says. RSV, influenza and Covid are all diseases that often re-occur and that can spread rapidly in the human body. “In older or immunocompromised patients at a particularly high risk when infected, this sort of medication could prove very advantageous, as it could aid in boosting the immune system before serious problems arise,” he explains.
Whether and when this therapy will be on the market remains to be seen. After all, it takes years to test and commoditise new drugs. “That said, we’ve now demonstrated for the first time that the idea of a combined drug and vaccine, as it were, actually works,” Stellacci says. The researchers’ next step is testing Pam3FDA in a re-infection with the aim of learning more about the strength of the immunological memory induced by the active substance.






