All in sight, all under control
With their innovative robot-guided laser, the MIRACLE II team at the University of Basel and the University Hospital Basel are aiming to make minimally invasive surgery on bones and cartilage a reality. Their smart system of interacting robots—ranging from a large robotic arm to a tiny endoscopic laser scalpel—is already being tested for first applications in knee surgery. In addition, the researchers are working to develop 3D-printed bone implants that can be inserted using minimally invasive techniques.
Every patient undergoing an operation hopes for a simple intervention with no large incisions. In minimally invasive procedures, surgeons operate using endoscopes inserted through tiny incisions in the body, which is less traumatic for the patient and promotes swifter recovery. Since 2014, researchers in the MIRACLE project have been working to make minimally invasive surgery possible on bones. To this end, the team at the University of Basel and the University Hospital Basel are developing an integrated, smart system of robots that can cut bones gently and safely.
Four research groups in MIRACLE II
Based on the considerable success of the first project phase, the Werner Siemens Foundation has awarded the MIRACLE team funding for a further six years. As in the first phase, MIRACLE II will be led by Philippe Cattin, Professor of Image-Guided Therapy and Head of the Department of Biomedical Engineering (DBE) at the University of Basel and the University Hospital Basel. Cattin leads the project’s navigation group, which is tasked with preparing 3D-rendered models of CT scans for use in operations. The laser group, currently led by Azhar Zam, and the robotics group led by Georg Rauter are also remaining on board for the project’s second phase.
New to the team is clinician Florian Thieringer, an oral and cranio-maxillofacial surgeon at the University Hospital Basel, who also leads the DBE research group Medical Additive Manufacturing (Swiss MAM). The new co-leader of MIRACLE II is head of the fourth group in the project: “Smart Implants”. Indeed, bone incisions are only one element of bone surgery—after that, damaged sections of bone must be stabilised with a well-fitting implant. For this reason, Thieringer and his research group are seeking ways to customise bone implants for individual patients and insert them using the least invasive surgery techniques possible (see interview).

The integrated robot
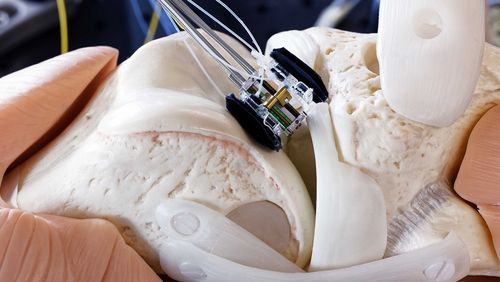
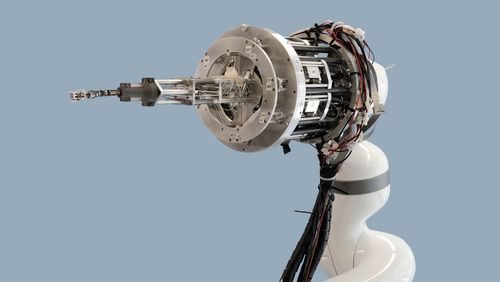
In the first project phase, Georg Rauter's team succeeded in developing the various robotic components, which were united in an integrated robot system in 2021. The base component, an approximately 1.5-metre robotic arm, is mounted on a guide rail next to or above the operating table so it can be moved into position over the part of the body requiring surgery. At the top of the robot arm are the motors powering the delicate surgical instruments to be inserted in the body: these include a flexible, six-jointed robotic endoscope that guides the laser to the surgery site, and the laser scalpel itself—a miniature robot that can latch on to the bone with two tiny “arms” and make incisions to the precision of one-tenth of a millimetre.
The researchers have also made great progress on the actual laser. When making incisions, it can now simultaneously monitor incision depth and differentiate between bone and soft tissue. Azhar Zam and his team of laser physicists made this development possible by using three different laser sources: one that cuts, and two that characterise tissue. The researchers synchronised the three light sources using a combination of shutters, mirrors and a controlling software program. Their next challenge is to miniaturise the system so that the laser beams can be channelled from a compact source through glass fibres into the endoscope tip.
First applications in knee surgery
The MIRACLE II team are already testing the application for use in knee surgery. “The knee is the largest joint in the body with the thickest bones,” explains Georg Rauter, head of the robotics group. “This makes it a good candidate for testing: if we can make minimally invasive incisions in knee bones, we can do it elsewhere, too.” The system may also prove useful in repairing knee cartilage. To develop such real-world applications, the researchers are working with various partners, including surgeons from the University Hospital Basel.
Meanwhile, the researchers are continually enhancing the capabilities of the various robotics components. In one development, the endoscope is capable of automatically following a specific point thanks to a tiny camera and a clever algorithm. In practice, the focal point is determined by the surgeons—in case the patient moves or is nudged during an operation, or in case the endoscope is required to observe the point from a different angle while also keeping it in constant focus.

Intuitive handling
It is not enough, however, that the robot system functions well: of equal importance is its handling. Specialists must be able to control the robot system with ease, despite its wide range of movement capabilities—a key concern for Georg Rauter and his team. Their solution lies in a novel intuitive kinematic system, a type of interactive lever on the robot arm. In the lab, postdoctoral researcher Nicolas Gerig demonstrates how the machine is used at the operating table. Using the lever, he guides the endoscope gently from the breast of a skeleton “patient” down to its left knee. Because the robot arm weighs a hefty eleven kilograms, the researchers have integrated a sophisticated software program that translates the readings from the remote control’s force sensors into the correct actions. Indeed, no surgeon has the strength to manoeuvre such a heavy apparatus unassisted during an operation.
Augmented reality leads the way
But the researchers are not stopping there: the MIRACLE II team have also integrated the robot into the augmented reality (AR) system developed by Philippe Cattin’s navigation group. The system renders patient CT scans as virtual 3D models; using special data goggles, physicians can then explore the models to plan surgical interventions. In the long term, the aim is to use these 3D images directly during an operation, which is why Cattin and his group are exploring ways to use a software program to project the three-dimensional CT scans automatically and precisely over the patient lying on the operating table. And the team have recently made a significant breakthrough: “It’s now possible to steer the robot directly from within the AR environment,” explains Cattin. “The surgeons have everything in sight: the robot-guided endoscope, the 3D-rendered CT scans and, of course, the patient.”
Text: Santina Russo
Photos: Oliver Lang