
The see-through body
Medical imaging techniques are used in almost every area of medicine. And researchers are continually discovering new ways of rendering the most minuscule structures in our bodies visible—as seen in a recent visit to the Werner Siemens Imaging Center in Tübingen.
A more fitting address for the Werner Siemens Imaging Center (WSIC) would be hard to imagine: Röntgenweg, a street the city of Tübingen named in 1956 in honour of Wilhelm Conrad Röntgen, the discoverer of X-rays. Röntgen is widely regarded as the founder of medical imaging, and it was his groundbreaking work in 1895 that first enabled doctors to look inside the human body without needing to cut it open.
In the meantime, numerous other non-invasive imaging techniques have been developed—also at WSIC, which opened its doors here in 2014. Today, under the leadership of Professor Bernd Pichler, fifteen research groups with a total of some one hundred and forty employees are currently working on—and further developing—many of these modern medical imaging methods. “Our innovative work is only possible thanks to the long-term funding provided by the Werner Siemens Foundation,” Bernd Pichler says. “Without WSS, our centre would have remained a small lab with five researchers.”
The Foundation’s support, which has recently been extended for another ten-year funding period, is instrumental in enabling the WSIC team to create the conditions for their cutting-edge research. And only institutions that generate first-rate findings have a chance of securing additional funding—and of growing. In this regard, WSIC researchers have achieved outstanding success: over the past twenty years, the group has raised more than one hundred million euros in funding. Indeed, in terms of financing, WSIC is looking at a pivotal year in 2025, when its renewal application for the German Research Foundation’s iFIT Cluster of Excellence is due. iFIT stands for “Image-guided and Functionally Instructed Tumor Therapies”, and WSIC is a leader in the cluster that will hopefully be funded with approximately eighty million euros over another seven-year period. “It’s also the only cluster of excellence for oncology in the whole of Germany,” Pichler says. “And most crucially, iFIT is of great strategic importance for us.”
Sleeper cells
Oncology is one of the research priorities at WSIC. Modern medical imaging devices are used in oncology to render tumours visible in a variety of ways. One of the most important areas here—which Bernd Pichler and his group have significantly shaped in recent decades—is the development of so-called tracers: substances with very low levels of radioactivity that are introduced into the body and take part in metabolic processes or bind to structures on the cell surface. Due to their radio-active labelling, the tracers—which are safe—can be detected using nuclear medicine techniques, including positron emission tomography (PET).
PET scans enable the researchers to differentiate between tissue phenotypes or metabolic processes in organs and cell phases. Regarding the latter, many tumour cells exist in what is known as a senescent state: although they no longer divide, these cells are still alive and can trigger the growth of other tumour cells. Pichler says, cancer therapies for treating solid tumours have been known to cause cells to enter a senescent state: “This is a double-edged sword—on the one hand they don’t proliferate anymore but cause non-senescent cells to trigger tumour growth even more. That’s why detecting these cells and finding the right moment to administer drugs that destroy them is critical.”
Pichler and his team have developed promising tracers to identify these senescent tumour cells: a phase I clinical trial has already been completed and the tracer selected for the study has proven to be safe for use in patients. A phase II trial is now underway and, as Pichler says, “it looks very good”. The researchers have submitted a related article to a top-tier scientific journal. But they aren’t stopping there—Pichler says his team have already developed senescence tracers that are three to five times more accurate than the version currently being tested in the trials.


Chemie und Pharmazie
Anna Junker verbindet nämlich Kenntnisse und Erfahrungen aus zwei Kernbereichen der Tracer-gestützten medizinischen Bildgebung: Chemie und Pharmazie. Das Pingpong zwischen diesen beiden Fächern begann bei ihr bereits mit der Studienwahl. Sie studierte in Münster Pharmazie – aber erst im zweiten Anlauf, wie sie erzählt. Aufgrund eines Missverständnisses beim Antrag für die Studienplatzvergabe bekam sie einen Pharmazie-Studienplatz in Halle zugeteilt. «Dorthin wollte ich aber nicht», sagt sie. Kurzerhand schrieb sie sich in Münster für Chemie ein, wo es noch freie Studienplätze gab.
Ihre Absicht war es, nach dem ersten Semester ins Pharmazie-Studium in Münster zu wechseln – was sie auch tat. «Allerdings gefiel mir die Chemie derart gut, dass mir der Wechsel schwerfiel», sagt sie. Bereut hat sie den Schritt zur Arzneikunde trotzdem nie – zumal sich im dritten Semester ein neuerlicher Seitenwechsel anbahnte. Sie erinnere sich noch gut, erzählt Anna Junker. «Ich sass in einer Chemievorlesung bei Professor Bernhard Wünsch und war begeistert. Ich sagte zu meiner Sitznachbarin: Das, was er macht, will ich auch tun.»
Bernhard Wünsch entwickelt sogenannte Liganden, chemische Verbindungen, welche Rezeptoren in Zellmembranen aktivieren oder blockieren können. Anna Junker promovierte bei ihm – mit einem Abstecher nach Japan – und entwickelte erste radiofluorierte Tracer-Moleküle. «Als mein erster PET-Tracer in einer Maus getestet wurde, war das ein Aha-Moment», sagt sie. «Erstmals sah ich eines meiner Moleküle in einem lebenden Organismus.»
Sie merkte, dass ihr die organische Chemie sehr gut gefiel – aber medizinisch-pharmazeutische Anwendungen ihr noch mehr zusagten. Bis sie ihr genaues Feld fand, dauerte es allerdings noch einmal einige Jährchen: Sie war zuerst Postdoc in der Gruppe von Professorin Christa Müller an der Universität Bonn, was eine enge Zusammenarbeit mit einer Pharmafirma beinhaltete. Danach ging sie mit einem Forschungsstipendium für ein Jahr an die National Institutes of Health (NIH) nach Bethesda in den USA zu Professor Kenneth Jacobson, einem der Vorreiter der Erforschung sogenannter Adenosin-Rezeptoren, die bei einer Vielzahl von Erkrankungen eine Rolle spielen. «Das war nicht Imaging, sondern medizinische Chemie», erzählt Junker.
Die nächste Station war wieder Münster, wo sie mit einem Postdoc-Förderprogramm die Möglichkeit bekam, eigenständig an Rezeptoren zu arbeiten, die bei Prostatakrebs eine Rolle spielen. Gleichzeitig bewarb sie sich erfolgreich für eine Förderung über das Emmy-Noether-Programm der Deutschen Forschungsgemeinschaft. Sie erhielt für eine Förderperiode von sechs Jahren 1,3 Millionen Euro. «Das war entscheidend», sagt Anna Junker. «Ich konnte meine eigene Forschungsgruppe aufbauen – und zum ersten Mal etwas durchatmen und längerfristige Forschungsfragen angehen.»
Vielversprechende Entdeckung
Das hat sie mit Erfolg getan, wie die Berufung zur Professorin in Tübingen zeigt. Ein eindrückliches Beispiel ist Junkers bisher vielversprechendste Entdeckung: ein PET-Tracer für ein Enzym namens CD73, den sie in Münster entwickelte und für den die Universität Tübingen inzwischen das Patent übernommen hat. CD73 wandelt vom Adenosintriphosphat (ATP) stammendes Adenosinmonophosphat (AMP) in Adenosin um. ATP ist der universelle Energieträger in Zellen, und damit eines der wichtigsten Moleküle überhaupt in lebenden Organismen.
«Doch ATP kann auch in den ausserzellulären Raum gelangen und ist dort ein Signalmolekül, welches das Immunsystem auf eine Gefahr oder eine Entzündung hinweist», erklärt Anna Junker. Adenosin ist genau das Gegenteil: Das Vorkommen dieses Moleküls bedeutet dem Körper: keine Gefahr, es müssen keine Immunzellen aktiviert werden! Extrazellulär wird ATP sehr schnell zu AMP abgebaut und durch CD73 zu Adenosin umgewandelt. Das nützen viele Krebszellen: «Alle soliden Tumore produzieren CD73 verstärkt», sagt Anna Junker. «Das führt dazu, dass sie sich richtiggehend in eine Adenosin-Wolke hüllen, die das Immunsystem des Körpers fernhält.»
Ihre Idee ist es, mit einem radioaktiv markierten CD73-Liganden die Abwehrstrategien von Krebszellen sichtbar zu machen – oder gar zu bekämpfen, wenn der Ligand den Umbau von AMP in Adenosin hemmt. Den ersten Punkt haben die Forschenden für Pankreas- und Brustkrebs bereits nachgewiesen. «Mit dem von uns entwickelten Tracer stellen wir diese Tumore im Tiermodell viel genauer dar als mit dem bisherigen Goldstandard», erzählt Junker.
Bis die Entwicklung ihren Weg in Patientinnen und Patienten findet, wird es noch ein Weilchen dauern. Doch Anna Junker ist optimistisch: «Die Infrastruktur hier in Tübingen ist hervorragend für die Translation vom Labor zur Patientenversorgung – es gibt nur wenige Standorte in Deutschland, die diesbezüglich derart gut aufgestellt sind.»
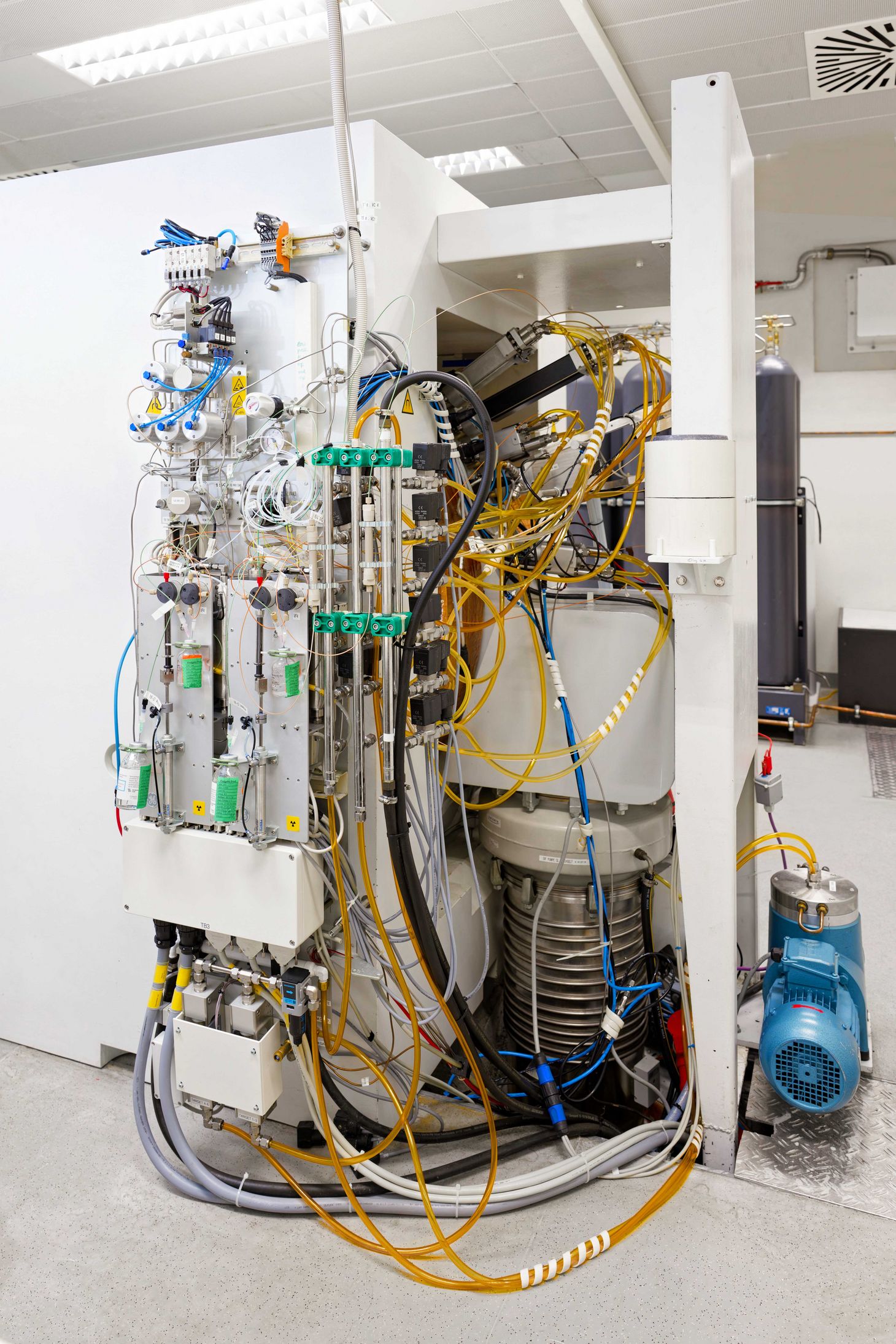
Tatsächlich: Ein kleiner Rundgang durch die Räumlichkeiten und Labore des WSIC lässt erahnen, welch breit gefächerte, hochkarätige und interdisziplinäre Forschung hier betrieben wird: Da gibt es Chemie- und Mikrobiologie-Labore. Es gibt Analytikgeräte für Reaktionskontrollen. Es gibt Labore, in denen die Tracer entstehen.
Die hochwertigsten und empfindlichsten Geräte befinden sich hinter verschlossenen Türen: teure, grosse Mikroskope und natürlich die PET-Scanner in den Imaging-Laboren. In ihnen wird untersucht, wie die Tracer sich in Geweben oder Versuchstieren verhalten. In diesen Räumen müssen selbst winzigste Verunreinigungen vermieden werden – es darf sie nur betreten, wer sich entsprechenden Reinigungsprozeduren unterzogen hat.
WSS competition for doctoral students
Conducting independent research is no easy task, especially at the outset of a research career. To help PhD students get off to a good start in their projects, the Werner Siemens Imaging Center (WSIC) organised a competition with funding from the Werner Siemens Foundation. During a week-long retreat, doctoral students had the opportunity to work in small groups to develop and present their ideas, including a financial plan. The winning team—Daniel Bleher, Eden Laing and Laura Kübler—received a grant of fifty thousand euros to pursue their proposal. “It’s fantastic to have the chance to plan a project from scratch,” Daniel Bleher says with evident satisfaction.
The trio convinced the jury with their clever idea of developing a tracer that indicates Porphyromonas gingivalis infections.
P. gingivalis is a key bacterium in cases of gum inflammation and chronic periodontitis. “In Germany, thirty to forty percent of all people will experience this kind of infection at least once in their lives,” Daniel Bleher explains. The bacteria’s impact, however, goes far beyond our mouths and oral health. Studies have linked P. gingivalis to chronic inflammation in the body as well as to neurological conditions and to poor prognoses for cancer patients.
“Our group is a dream team,” says Bleher, who is a PhD student in Professor Kristina Herfert’s group, where he develops tracers that detect structures in the brains of patients with Parkinson’s or related diseases. Eden Laing, who belongs to the group of Privatdocent Nicolas Bézière, is working on her dissertation in the area of infection imaging. And Laura Kübler, who is now a postdoc in Professor André Martins’s group, contributes her experience in tumour imaging.
The three are working on their joint project alongside their day-to-day research. “It demands an extra effort from all of us,” Daniel Bleher says. “But when given a chance like this, there’s no question that we’ll be putting in the work.” The junior researchers have already met with success: they’ve synthesised several compounds that have potential in radioactive labelling. “We’re also cultivating the inflammatory bacteria for the study, which is actually quite difficult because they only grow in an oxygen-free environment.” Their aim is to test the radiolabelled compounds in the bacteria and then later in diseased tissue. “If all goes well,” Daniel Bleher says, “the findings may result in an initial publication and the possibility to continue pursuing the idea in a larger project.”
He believes the WSIC competition for PhD students is unique, adding that it was certainly the first one he had ever heard of, and that PhD students responded to the event with huge interest. “It would be fantastic if something similar could be held again.”
Managing data overload
Just a brief tour of the centre and its labs provides ample evidence of the depth, breadth and excellence of the interdisciplinary research conducted at WSIC. There are chemistry and microbiology labs, analytical devices for reaction controls and labs for designing tracers.
The premium—and most sensitive—devices are located behind closed doors: large, costly microscopes and, of course, the PET scanners in the imaging labs used to observe the tracers in tissues or lab animals. In all the facilities, it’s critical to avoid even the most minuscule impurities, and researchers must first undergo a complex cleansing procedure before they’re permitted to enter.
One rather nondescript little room houses a key component in the research conducted at WSIC: powerful computer stations used for analysing data gathered in the experiments. Despite their many differences, all imaging techniques generate massive amounts of data, and researchers must rely on specialised software programs, memory cards and large computers in order to come to terms with the abundance of information. “Dealing with all the data is one of our biggest challenges,” Bernd Pichler says. “Because the key issue in future is that we’ll no longer be simply working with multi-modal systems—we’ll be working on multiple scales.”
In practice, this means not just combining techniques like PET, MRI and CT, but merging microscopic and macroscopic studies: for example, scanning the entire body for metastases—at a high-spatial resolution. In addition to the sheer volume of data generated, the information is incredibly complex and comes in a wide spectrum of formats.
Tracers with faster tissue distribution
Pichler is convinced that this ability to establish connections across various body organs will play an ever-greater role in examinations and diagnoses. “We’ve repeatedly seen that immunotherapies are effective only in some patients,” Pichler says. “By studying key organs and tissues of the immune system—the spleen or bone marrow, for example—we can help uncover the links.”
On top of this, the team will also continue their efforts to drive innovation in individual medical imaging techniques. For instance, the Tübingen researchers are currently working on nanobodies—PET tracers created on the basis of antibody fragments so tiny that they can distribute better and faster throughout the body, where they can be used for medical imaging.
“We’ve been studying these nanobodies for around five years—as one of just a few research groups in the world,” Bernd Pichler says. And that with very satisfying results. Recently, WSIC saw the foundation of its first spin-off company, immunAdvice, where researchers are using nanobody tracers to visualise immune cells in the body with the aim of assessing an immunotherapy’s success.
This example demonstrates two points. First, the imaging experts in Tübingen are in no danger of running out of ideas. Second, their research is consistently geared towards bringing tangible benefits to patients as swiftly as possible.







